Mucormycosis Black Fungus: Symptoms & Treatment

Mucormycosis is a rare but serious fungal disease and if left untreated may turn fatal.
Its spores are usually found in dust, soil and enter the inside body through
- Inhalation of spores through the nose and paranasal sinuses
- Direct Inoculation through cut wounds, Gum disease especially bleeding gums
- Mucormycosis is not contagious that is it doesn’t spread from person to person
In COVID-19 patients there is a significant increase in the incidence of secondary infections, both fungal and bacteria which is probably due to
- Immune dysregulation due to coronavirus
- Widespread use of steroids and monoclonal antibodies
- The use of broad-spectrum antibiotics as part of the COVID-19 regime may lead to the exacerbation of preexisting fungal diseases.
Table of Contents
Causes of Mucormycosis
The chief cause for mucormycosis in COVID patients are
Steroids
Overuse of steroids when not needed or used in very high dosage.
Uncontrolled Diabetes
Just diabetes is a small risk factor but high blood sugar and uncontrolled diabetes is a high-risk factor.
The patients who are diabetic and are on steroid therapy should monitor sugar levels stringently as steroids also increase blood sugar levels.
If the patient is on oral hypoglycemics should not hesitate to switch to insulin therapy on the doctor’s advice.
Injudicious use of antibiotics
Unnecessary use of antibiotics should be avoided, as once the bacteria are killed fungal particle come in
Poor Oral Dental Hygiene

Poor dental hygiene also plays a major role in mucormycosis disease progression
Unhygienic use of oxygen therapy:
The use of oxygen concentrators, tubes, or mask that are not clean or the water used to humidify oxygen or the vessel used is not clean and can cause fungal particles to grow in.
Comorbid conditions:
Patient those are already on immunosuppressive medications, transplant patients or patients having cancer or undergoing chemotherapy are at higher risk of getting mucormycosis
Signs and Symptoms of Mucormycosis

Mucormycosis could be a killer disease one can lose vision, a portion of the jaw, or even life.
It is mandatory to diagnose it at the earliest to prevent serious outcomes
General Symptoms
The main symptoms of Mucormycosis are
- Headache
- Facial pain, Pain in Cheekbones
- Numbness of face
- Swelling on face or mouth
- Nasal Congestion
- Nasal Discharge ( blackish/ bloody)
- Pain around Eyes
- Redness of eye
- Watering of eye
- Loosening of teeth
- Toothache
- Blackening of gums, Palate, or bridge of the nose
- Chest pain, worsening of breathing problems
So those are warning signs that you must consult an Oral &Maxillofacial Surgeon, ENT Specialist Eye Specialist, Dentist or Pulmonologist
Neurological Symptoms
Once it goes inside brain through nose or sinuses neurological symptoms occurs
- Brain inflammation
- Headache
- Fits
- Forgetfulness
- Optic nerve involvement
- Double Vision
- Blindness
- Brain Abscess
With these symptoms visit a Neurosurgeon at the earliest.
How To Prevent Mucormycosis
- Use a mask if you are visiting a dusty construction site
- Wear shoes, gloves, and protective wear while handling soil, manure, or moss
- Maintain personal hygiene and oral hygiene.
What Should Covid Patient Do to Prevent Black Fungus
- Control Diabetes
- Monitor Blood Glucose level post covid discharge
- Use steroid therapy judiciously, Take steroid medication under the guidance of your doctor only
- Use clean sterile water for humidification in oxygen concentrators and cylinders
- Change oxygen mask and tubing periodically
- Use antibiotics only on doctors prescription do not overuse antibiotics
- Do not ignore the warning signs
- Do not consider all cases of the blocked nose as bacterial sinusitis particularly in covid patients or the patients on immunomodulators and steroids
Investigations Required to Diagnose Mucormycosis
- KOH staining, microscopy, Culture. MALDITOF for detecting fungal etiology.
- CT Scan
- MRI
Treatment of Mucormycosis Infection
- Control Diabetes
- Reduce steroids with the aim to discontinue rapidly
- Surgical Debridement of involved bone
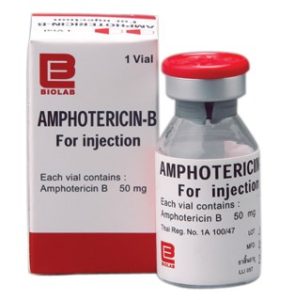
- Amphotericin B infusion
- Antifungal therapy for at least 4weeks to 6 weeks
Sources:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3286196/
https://en.wikipedia.org/wiki/Mucormycosis